
Executive Summary
In early 2025, the executive leadership of a major multi-site healthcare network with 15 facilities across four regions met to tackle a pressing issue: revenue growth had stagnated despite strong clinical results and an increase in patient numbers. Behind the success of its high-quality care, operational shortcomings and fragmented systems were impacting financial performance. The organization was facing significant revenue leakage, disparate RCM and CRM systems, and prolonged billing cycles.
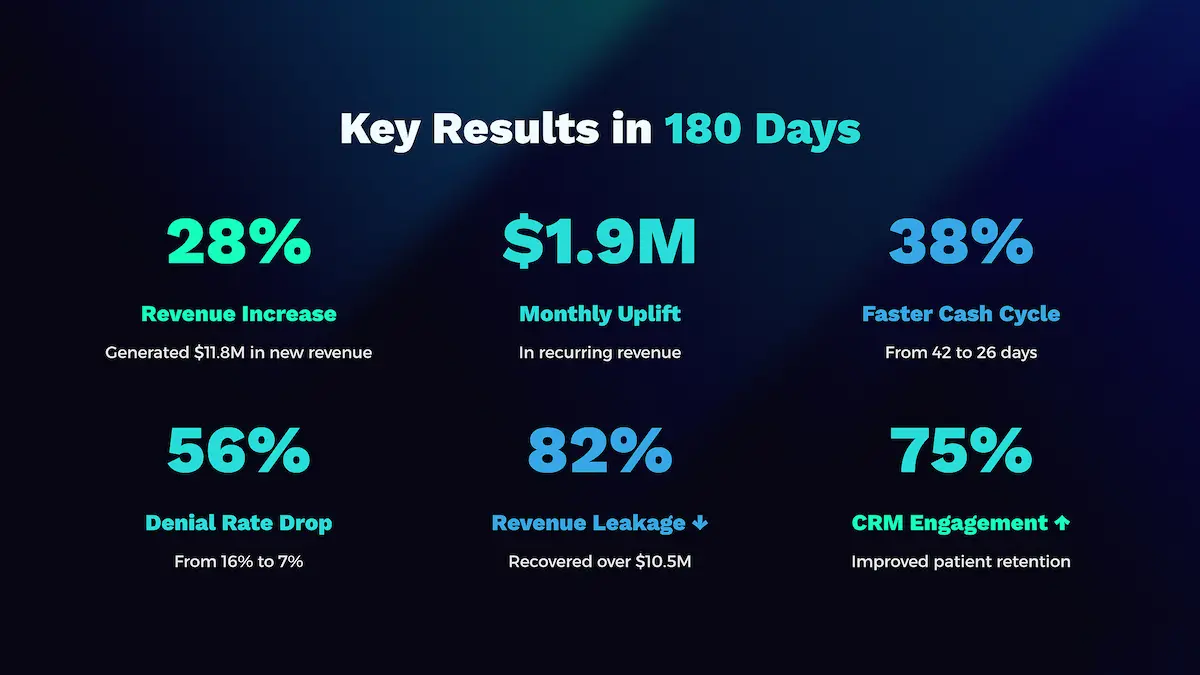
OTLEN was brought on to spearhead a complete overhaul of the network’s revenue operations. By implementing its AI-powered RevOps platform, OTLEN integrated RCM and CRM workflows, automated billing and referral management, and leveraged predictive analytics to fine-tune performance. The impact was significant within just 180 days: a 28% increase in revenue, which generated $11.8 million in new revenue. This initiative marked a strategic shift to intelligent, data-centric operations that harmonized clinical excellence with financial stability.
At a Glance
- The Client: A leading multi-site healthcare network with 15 facilities across four regions, serving over 2 million patients annually.
- The Challenge: Significant revenue leakage, disparate RCM and CRM systems, a 16% claim denial rate, and a prolonged 42-day billing cycle despite strong clinical outcomes.
- The Solution: OTLEN’s AI-powered RevOps platform to unify RCM and CRM, coupled with predictive analytics.
At a Glance
The Client
Leading multi-site healthcare network with 15 facilities across four regions serving over 2 million patients annually.
The Challenge
Significant revenue leakage, disparate RCM and CRM systems, 16% claim denial rate, and prolonged 42-day billing cycles despite strong clinical outcomes.
The Solution
OTLEN’s AI-powered RevOps platform to unify RCM and CRM, coupled with predictive analytics.
Strategic Imperative: Laying the Groundwork for Scalable Growth
By late 2024, the healthcare network faced a stark reality: financial stability was diminishing. Operational expenses had climbed 9% year-over-year, and disconnected systems were leading to millions in annual losses. The leadership team recognized that superficial solutions were no longer adequate. They needed a fundamental change to regain financial stability and pave the way for sustainable expansion.
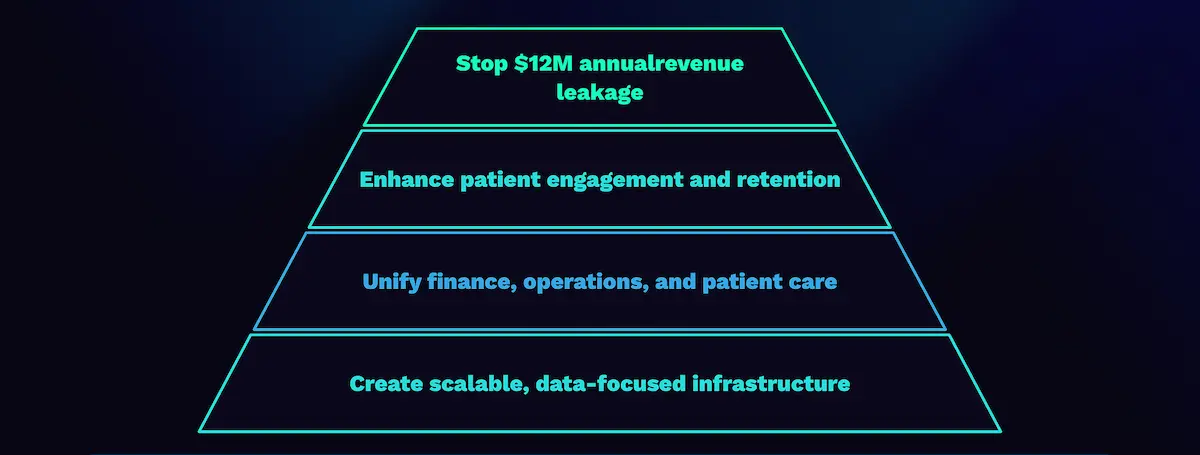
They set four main goals:
- Stop the $12M in annual revenue leakage and billing inefficiencies.
- Enhance patient engagement and retention through better referral conversions and follow-up.
- Unify finance, operations, and patient care under a single RevOps strategy.
- Create a scalable, data-focused infrastructure to support future moves into value-based care.
Internal assessments revealed disconnected systems and reactive procedures leading to millions in annual losses from missed revenue and administrative inefficiencies. This was not just about fixing revenue; it was about transforming the organization’s entore way of operating.
The Solution: A Three-Phase Implementation
OTLEN’s work started with an in-depth analysis, working directly with staff to grasp the practical challenges. To tackle the issues, OTLEN rolled out its AI-powered RevOps platform in three carefully planned stages.
- Phase One: RCM Intelligence: OTLEN implemented real-time analytics for billing operations. Within 30 days, the system identified $12M in missed billing opportunities. By day 90, claim recovery rates had increased by 20%.
- Phase Two: CRM Automation: Manual tracking was replaced with smart engagement plans customized to patient profiles. This improved patient retention by 17% and increased referral conversions by 25%, generating $3.2M in new patient revenue in the first quarter.
- Phase Three: Predictive Modeling: AI-driven predictions were introduced to revolutionize revenue forecasting. This improved billing accuracy by 30% and reduced payer response times by 10 days, accelerating cash flow.
The Solution: Three-Phase Implementation
Phase One: RCM Intelligence
Implemented real-time analytics for billing operations, highlighting undercoding and claim denials. Within 30 days, identified $12M in missed billing opportunities. By day 90, claim recovery rates increased by 20%.
Phase Two: CRM Automation
Replaced manual tracking with smart engagement plans customized to patient profiles. Patient retention improved by 17%, referral conversions increased by 25%, generating $3.2M in new patient revenue in the first quarter.
Phase Three: Predictive Modeling
Revolutionized revenue forecasting with AI-driven predictions. Billing accuracy improved by 30%, payer response times reduced by 10 days, accelerating cash flow and reducing administrative work.
Results and Impact
In just 180 days, the organization underwent a significant transformation in both its financial and operational areas, achieving a 28% rise in total revenue.
Success Highlights
OTLEN’s AI-powered RevOps platform consolidated RCM and CRM data into a single, intelligent layer, offering real-time visibility and cutting data reconciliation time by 65%.
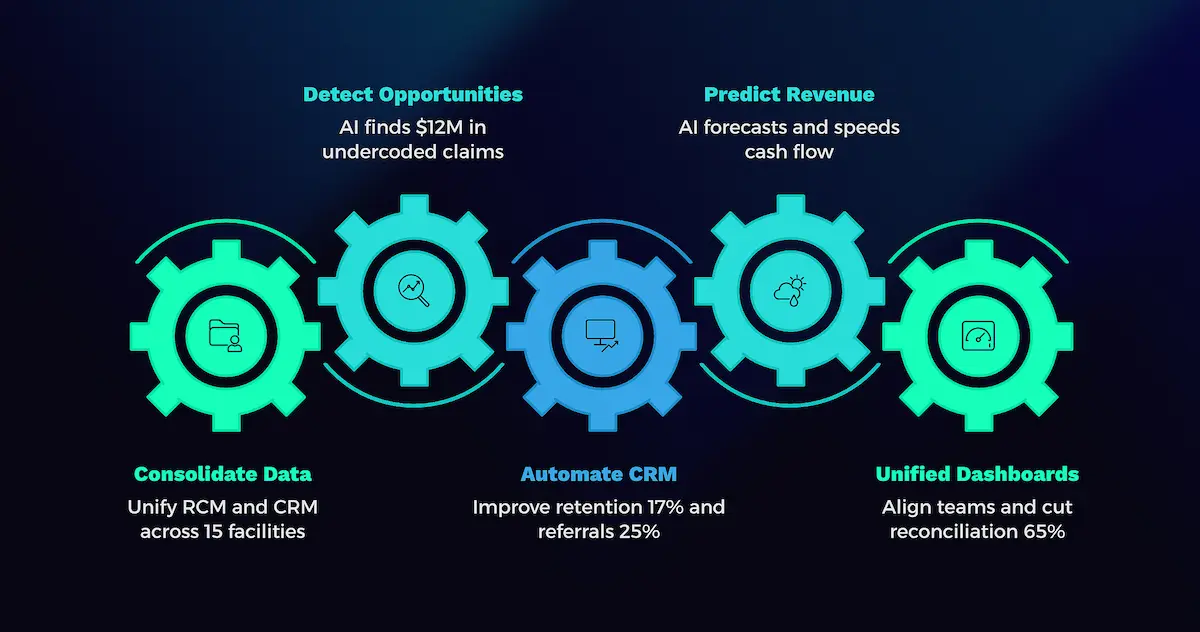
AI algorithm pinpointed $12 million in undercoded claims and other missed billing opportunities in the initial 90 days CRM automation improved patient retention by 17% and increased referra conversion by 25% adding $3.2 million in new patient revenue. Unified dashboard brought departments into alignment, imporving interdepartmental decision-making speed by 40%.
Financial & Operational Impact
The financial improvement was swift and lasting. Manual billing tasks were replaced with automated systems, diminishing the likelihood of human error and allowing staff to concentrate on more strategic work.
-
Financial Performance Uplift: The network saw $1.9M in monthly revenue gains, a 29% enhancement in billing accuracy through AI-driven audits, and a 3.5 percentage point increase in net revenue margin, reversing a two-year decline.
-
Operational Proficiency Gains: Automated systems, smoother patient follow-ups through CRM integration, and unified dashboards led to a 17% rise in staff productivity and immediate access to performance data.
Financial Performance Uplift
$1.9M monthly revenue gains from more accurate billing and better patient retention.
29% enhancement in billing accuracy through AI-driven audits.
Net revenue margin increased by 3.5 percentage points, reversing a two-year decline.
Operational Proficiency Gains
Manual billing tasks replaced with automated systems.
CRM integration facilitated smooth patient follow-ups and 17% rise in staff productivity.
Unified dashboards provided immediate access to performance data.
Cultural & Strategic Transformation
The most significant transformation was in the collective mindset. The organization moved from reactive billing to a proactive revenue strategy founded on data, responsibility, and collective ownership.
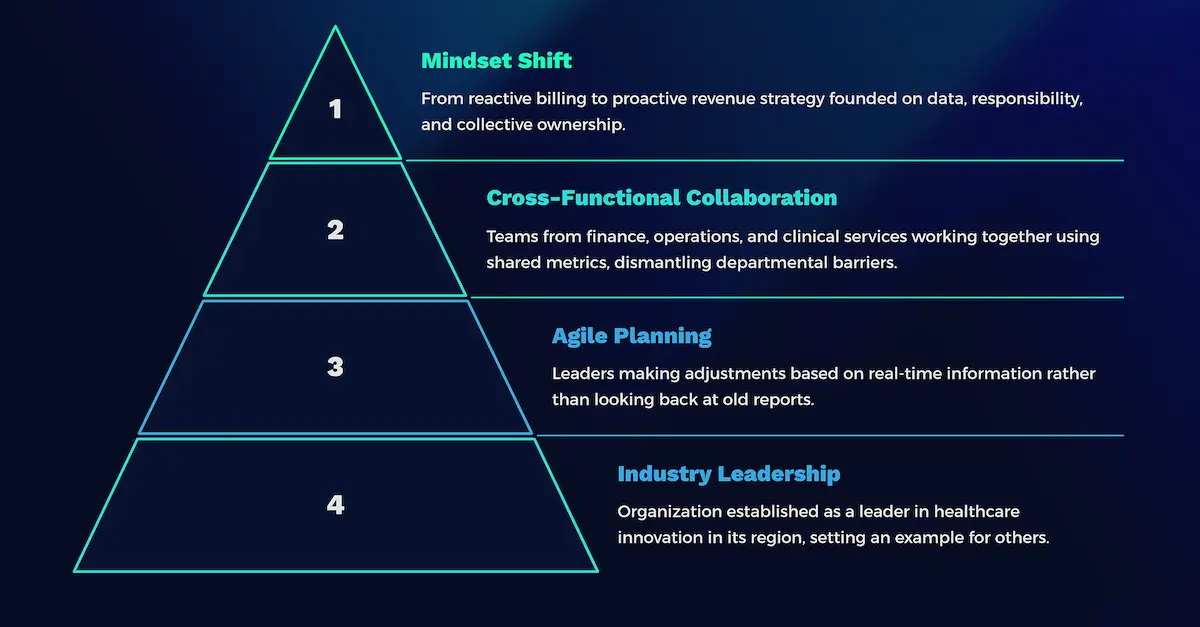
A Blueprint for Success
The transformation was more than just a technology update; it was a complete strategic overhaul. It provided a repeatable model for success:
- Integrate RCM & CRM: Break down data barriers to reveal practical insights.
- Apply AI Analytics: Find and prioritize revenue opportunities.
- Unify Departments: Bring all teams together under a single RevOps strategy with shared dashboards.
- Continuous Improvement: Track results in real time and expand successful projects.

Future Roadmap
With a solid foundation now established, OTLEN is expanding the scope of the RevOps platform into new areas to build on this success:
- Supply Chain & Workforce Analytics to better manage costs and optimize staffing.
- Patient Experience Integration to create more personalized outreach.
- Predictive Staffing Models to reduce overtime expenses.
- Value-Based Care Optimization to maximize revenue from new payment structures.
Supply Chain & Workforce Analytics
Better manage costs and optimize staffing.
Patient Experience Integration
Create more personalized outreach and increase satisfaction levels.
Predictive Staffing Models
Reduce overtime expenses and make scheduling more efficient.
Value-Based Care Optimization
Maximize revenue from new payment structures through strategic alliances.
