The multi-billion-dollar headache of claim denials continues to plague the healthcare and biotech industries, creating a significant drain on resources and revenue. For too long, revenue cycle management (RCM) has relied on a reactive approach, with clearinghouses flagging denials only after they occur. This post-submission scramble is no longer sustainable. The future of a healthy revenue cycle lies upstream, where Artificial Intelligence (AI) is predicting, preventing, and optimizing claims before they ever have a chance to be denied.
Claim denials represent a significant and escalating challenge for healthcare providers. The administrative cost to rework a single denied claim averages around $25, with studies showing this expense can reach as high as $118 per claim. This financial strain is compounded by a rising tide of denials. Recent reports indicate an upward trend in denial rates, with initial denials reaching 11.8% in 2024, an increase from 10.2% in previous years. A 2024 survey further highlighted this issue, with nearly three-quarters of responding healthcare staff reporting an increase in claim denials. The collective cost of battling these denials is substantial.
In 2022, U.S. hospitals and health systems spent an estimated $19.7 billion annually to manage denied claims. More recent data from early 2025 suggests this figure has surged to over $25.7 billion.
The Status Quo: Clearinghouses and Their Constraints
A clearinghouse acts as an intermediary, scrubbing claims for basic errors before they are submitted to payers. This is a crucial function that helps reduce immediate rejections for simple mistakes. However, this model is inherently reactive. Denials are identified after the fact, forcing RCM teams into a constant cycle of rework and appeals.
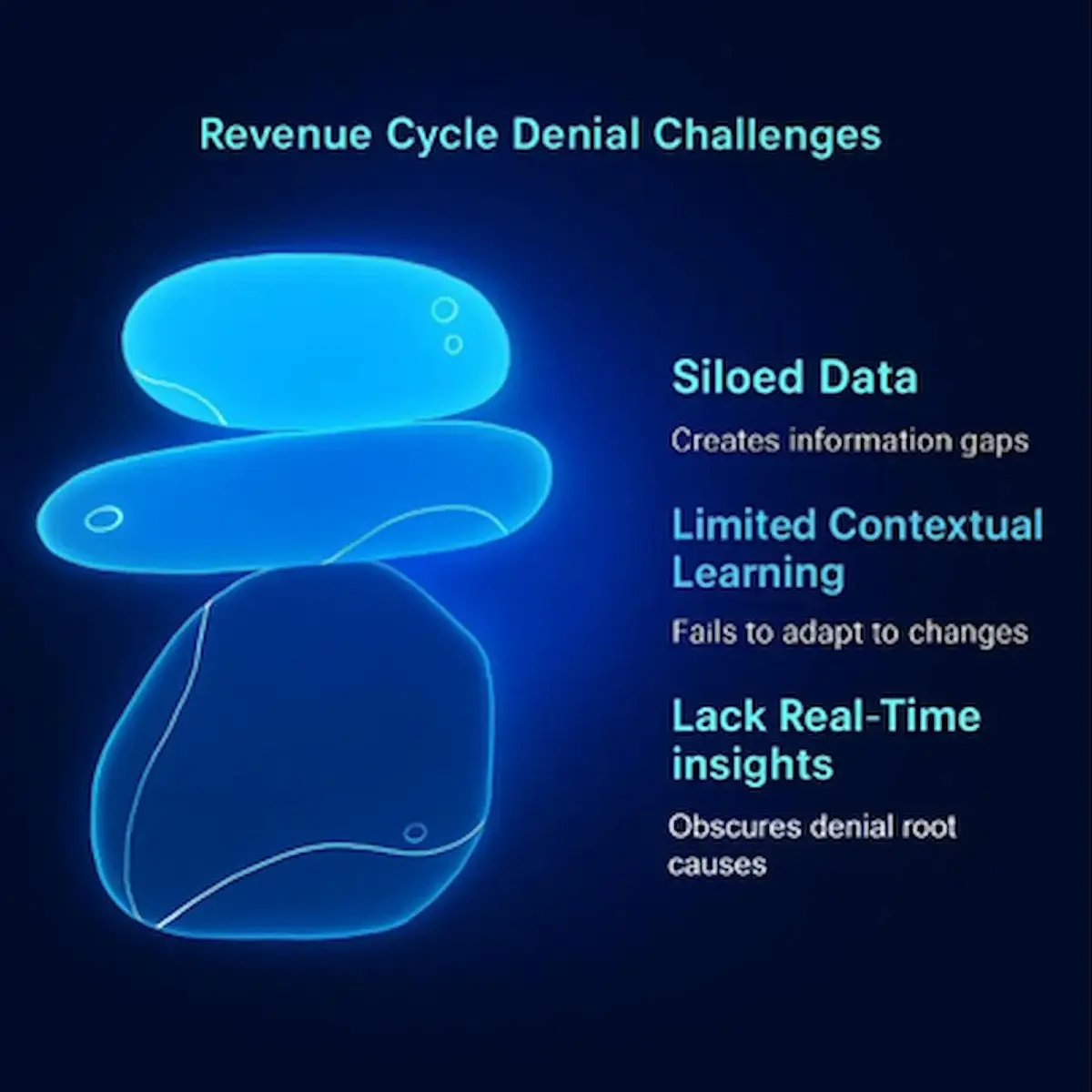
The primary gaps in this traditional approach are significant:
- Lack of Real-Time Insights: Clearinghouses typically don’t provide deep, real-time analytics into the root causes of denials across different payers and patient populations.
- Limited Contextual Learning: They often lack the sophisticated learning capabilities to adapt to the ever-changing and complex rules of individual payers.
- Siloed Data: The data from clearinghouses is often not seamlessly integrated with electronic health records (EHRs) and billing platforms, creating information gaps.
AI-Driven Denial Prevention: 3 Transformative Approaches
AI is moving denial management from a reactive chore to a proactive strategy. By leveraging predictive analytics and intelligent automation, healthcare and biotech organizations can now prevent denials before they happen. Here are three of the most transformative AI-driven approaches:
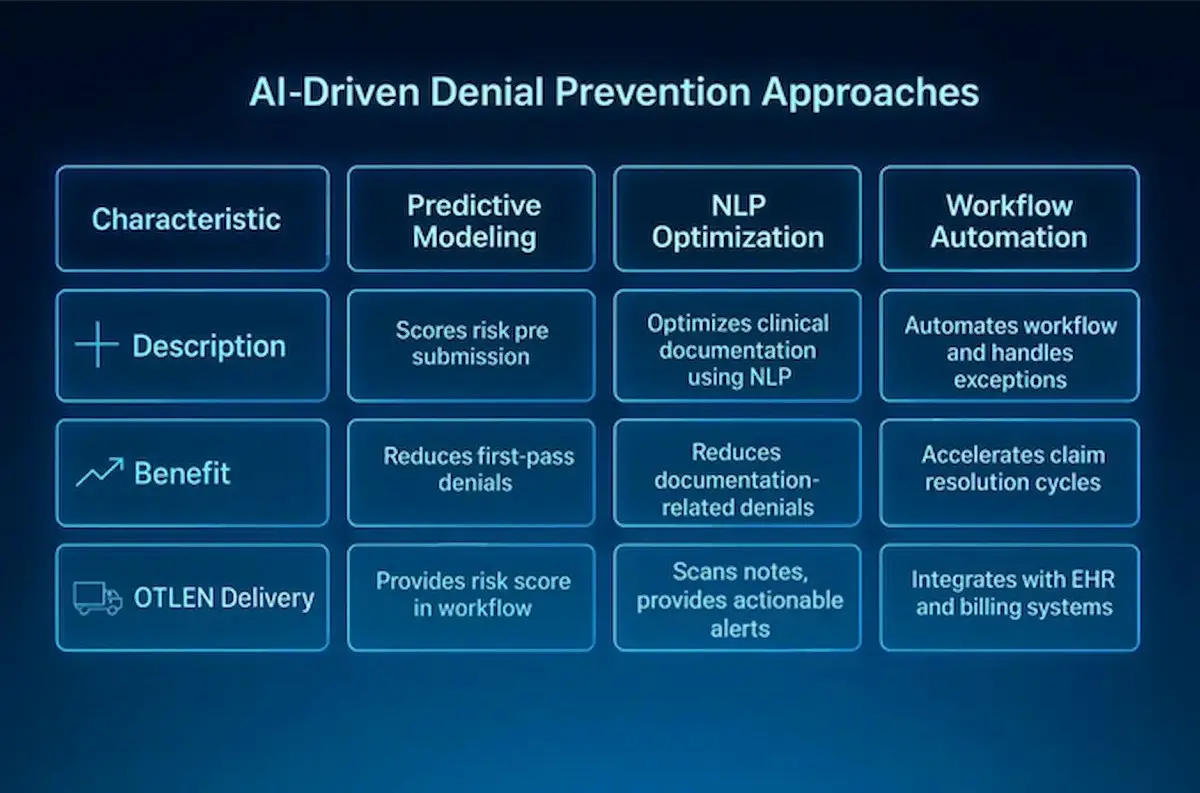
1. Predictive Modeling for Pre-Submission Risk Scoring
Imagine knowing the likelihood of a claim being denied before you even hit “submit.” This is the power of AI-powered predictive modeling. By analyzing vast amounts of historical claims data, machine learning algorithms can identify high-risk claims in real-time. These models can pinpoint payer-specific denial patterns, flag potential ICD/CPT code mismatches, and identify documentation gaps that are likely to trigger a denial. This proactive risk scoring allows billing teams to correct errors pre-submission, with some systems shown to reduce first-pass denials by up to 15%.
- How OTLEN Delivers: OTLEN’s predictive engine analyzes your historical claims and payer data to provide this pre-submission risk score directly within your existing workflow.
2. NLP-Powered Clinical Documentation Optimization
A significant portion of denials stem from a lack of medical necessity or insufficient clinical documentation. Natural Language Processing (NLP), a branch of AI, is tackling this challenge head-on. NLP tools can “read” and analyze unstructured clinical notes from physicians, providing real-time feedback to both coders and clinicians. These systems can identify when documentation is vague or missing key details required by payers and prompt for clarification, reducing documentation-related denials by over 20%.
- How OTLEN Delivers: OTLEN’s platform leverages advanced NLP to scan clinical notes, providing coders and clinicians with actionable alerts to strengthen documentation before claim creation.
3. Intelligent Workflow Automation and Exception Handling
AI is also revolutionizing the operational flow of the revenue cycle. Intelligent workflow automation can triage claims based on their denial likelihood, automatically routing high-risk claims for expert review while allowing low-risk claims to proceed without manual intervention. These AI systems can integrate directly with EHRs and billing platforms, creating a seamless flow of data and reducing the manual, repetitive tasks that bog down RCM teams. This not only accelerates claim resolution cycles by 30% or more but also makes compliance more scalable and reduces the chance of human error.
- How OTLEN Delivers: OTLEN integrates seamlessly with your EHR and billing systems, automating claim routing and exception handling to focus your team’s expertise where it’s needed most.
Case Study Snapshot: Schneck Medical Center
The power of predictive modeling (Approach #1) is not just theoretical. A real-world example of AI’s impact comes from Schneck Medical Center. By implementing an AI-powered predictive denials solution, they were able to gain deeper insight into the origins of denials and take preventative action before claims were submitted. Within just six months, Schneck reduced their denials by an average of 4.6% each month. The time it took to rework flagged claims also saw a dramatic decrease. This case highlights the tangible return on investment in both time and revenue that AI can deliver.
Strategic Takeaways for RCM Leaders
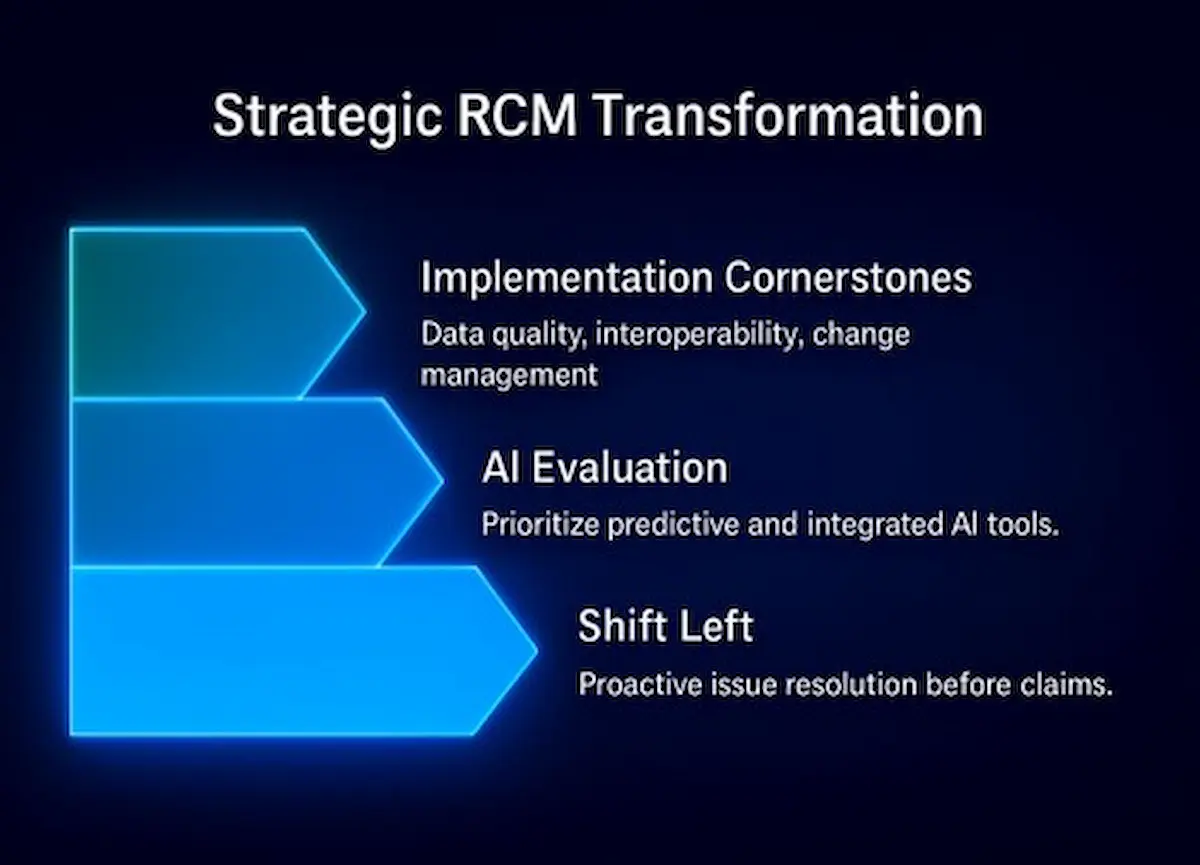
The message for revenue cycle leaders is clear: the focus must shift from denial management to denial prevention. Here are key considerations for embracing this new paradigm:
- Shift Left in the Revenue Cycle: Proactively addressing potential issues before claims are submitted is paramount to improving financial outcomes.
- Evaluate AI Tools for Upstream Impact: When considering AI solutions, prioritize those that offer predictive capabilities and can be integrated early in the workflow.
- Focus on Implementation Cornerstones: Successful AI implementation hinges on high-quality data, seamless interoperability with existing systems like EHRs, and a robust change management strategy to ensure user adoption.
Conclusion
Continuing to rely solely on clearinghouses for denial management is an outdated and costly strategy. AI is not just another tool; it’s a strategic enabler that empowers healthcare and biotech organizations to move beyond reactive problem-solving. By embracing AI-powered predictive analytics, NLP-driven documentation improvement, and intelligent automation, RCM leaders can build a more resilient, efficient, and profitable revenue cycle. Take the first step toward a healthier revenue cycle. See how OTLEN can help you shift left.
