From Silos to Synergy: How AI Unifies Data for a Holistic RevOps Approach
The modern healthcare revenue engine often sputters, not due to a lack of effort, but because of hidden friction points between clinical care and financial outcomes. These unseen barriers stall growth, diminish patient trust, and ultimately erode profitability.
Consider a common scenario: a patient is reassured that a crucial procedure is approved, only to face a surprise denial weeks later. This isn’t just an administrative hiccup; it’s a symptom of a deeper systemic issue where vital information shared at the front desk doesn’t seamlessly reach the billing department, leading to a fragmented understanding of the patient’s financial journey. The front desk, the clinic, and the back office frequently operate on separate islands, each with its own systems, processes, and data. This fragmentation creates data silos, preventing a cohesive understanding of the patient’s journey—both clinically and financially.
OTLEN understands this challenge intimately. We recognize that true progress lies in bridging these islands, creating a single source of truth that informs every decision. Artificial Intelligence (AI) serves as this crucial bridge. By unifying disparate data, AI transforms a fragmented landscape into a seamlessly integrated ecosystem.
Defining Revenue Operations (RevOps) for Healthcare
RevOps is more than just a contemporary term for Revenue Cycle Management (RCM); it represents a fundamental organizational strategy. It’s about aligning traditionally disparate clinical and administrative departments—from patient access and clinical documentation to billing and collections—around a singular, overarching goal: delivering a seamless, positive patient financial journey that ultimately drives sustainable revenue growth.
In the conventional model, departments often operate with distinct, often isolated objectives. Patient Access teams might focus solely on efficient registration, while the Billing department prioritizes collections. While individually necessary, this approach frequently overlooks the interconnectedness of their roles. RevOps, conversely, fosters a unified mission. Every team member becomes accountable for preventing denials, optimizing the patient’s financial experience, and ensuring the accurate capture of revenue. This shift from departmental goals to a unified mission is pivotal for modern healthcare enterprises.
The Silo Effect: How Disparate Data Cripples Healthcare Growth
The impact of fragmented data within healthcare organizations is profound, leading to inefficiencies and direct financial losses. Complex administrative processes, worsened by disconnected data, contribute to an estimated $265.6 billion in waste annually within the US healthcare system. This waste stems from issues like unnecessary paperwork, billing errors, and poor coordination between payers and providers.
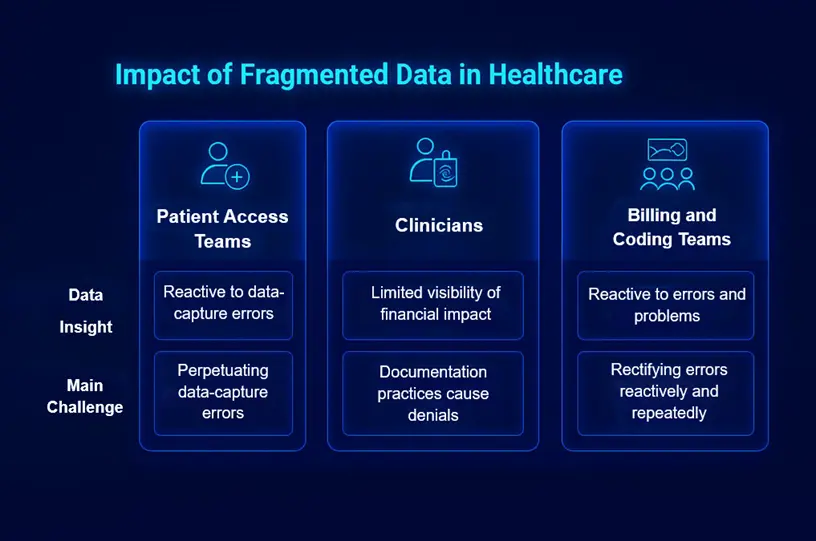
- Front-End Myopia: Patient Access teams, often lacking real-time insights into common denial reasons stemming from the back-end, inadvertently perpetuate the same data-capture errors. Without a feedback loop from billing and claims, they operate in a reactive mode, unaware of how their initial inputs cascade into downstream problems.
- Clinical Blind Spots: Clinicians, focused primarily on patient care, often lack visibility into the financial implications of their documentation practices. Seemingly minor omissions or ambiguities in clinical notes can inadvertently trigger denials, underpayments, or prolonged appeals processes, despite the high quality of care provided.
- Back-Office on the Back Foot: Billing and coding teams frequently find themselves in a perpetually reactive state. They spend an inordinate amount of time trying to rectify problems—such as incorrect insurance information or insufficient prior authorizations—that could and should have been caught proactively at the point of service or during scheduling.
The cumulative effect of these challenges is severe: rising denial rates, increasing accounts receivable (A/R) days, escalating administrative costs, profound patient frustration, and an unpredictable cash flow that hinders strategic planning and investment. These are not merely operational inconveniences; they directly impact the financial health and growth trajectory of the organization.
The AI Intervention: Forging a Single Source of Truth for Healthcare
The complexity of healthcare data—spanning electronic health records (EHR), practice management (PM) systems, and revenue cycle management (RCM) platforms—presents a formidable challenge for unification. This is precisely where AI delivers transformative value.
AI technologies act as the ultimate data orchestrator. They are engineered to seamlessly integrate and centralize information from these disparate systems, breaking down historical barriers and creating a cohesive, accessible data repository. Imagine AI as a sophisticated translator, speaking the unique language of each system and consolidating their insights into a universal lexicon.
Beyond mere aggregation, AI excels at automated data hygiene and enrichment. It proactively identifies and rectifies inconsistencies, redundancies, and errors within patient records. For instance, AI can automatically verify insurance eligibility in real-time, cross-reference patient demographics across systems, and flag potential discrepancies that human review might miss. This ensures that the foundational data upon which all financial decisions are made is accurate, complete, and reliable.
The result of this sophisticated integration and refinement is the creation of a 360-degree patient view. This comprehensive profile melds clinical history with financial data, insurance information, communication preferences, and payment history into a single, dynamic record. This unified perspective is not merely a convenience; it is the bedrock of a truly seamless patient journey, enabling informed decisions that benefit both the patient and the organization.
From Data to Decisions: AI-Powered Synergy in Action
With a unified data foundation established by AI, healthcare organizations can transition from reactive problem-solving to proactive, intelligent decision-making.
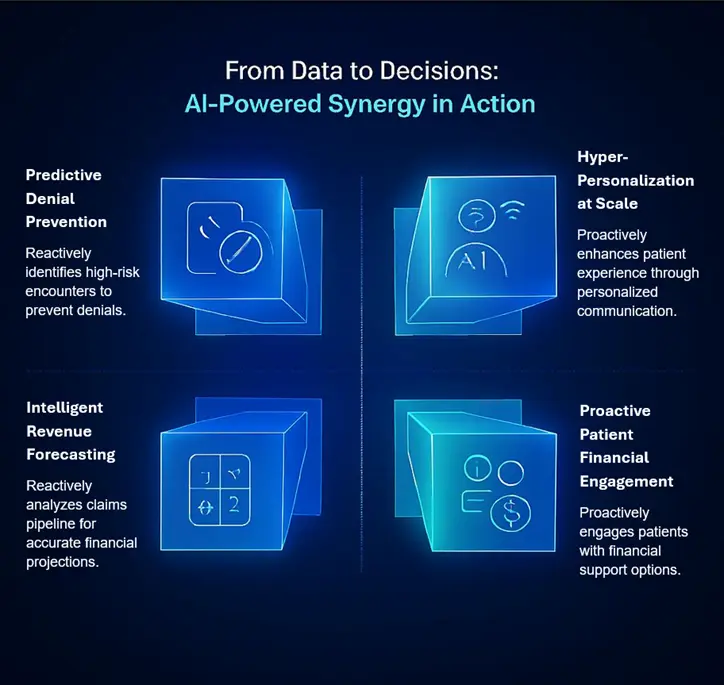
- Predictive Denial Prevention: AI’s analytical power is transformative here. By continuously analyzing the unified dataset—including historical denial patterns, patient demographics, procedure codes, and payer requirements—AI can identify a high-risk encounter at the very first touchpoint, such as scheduling. If a patient is scheduled for a procedure commonly denied by their insurer due to a specific pre-authorization requirement, AI flags this immediately. This empowers staff to address and resolve the issue weeks before service delivery, dramatically reducing the likelihood of a denial.
- Intelligent Revenue Forecasting: Traditional revenue forecasting often relies heavily on historical data, which can be a lagging indicator. AI moves beyond this limitation by analyzing the real-time health of the claims pipeline. It can assess the likelihood of payment for open claims, identify potential bottlenecks, and factor in current payer trends and policy changes. This provides far more accurate and dynamic cash flow projections, enabling more reliable financial planning and resource allocation.
- Proactive Patient Financial Engagement: Understanding a patient’s financial situation is critical for positive outcomes. AI can analyze a patient’s unified record to proactively identify those who might struggle with out-of-pocket costs. Based on their historical payments, insurance coverage, and the estimated cost of care, AI can trigger a personalized outreach. This might involve offering a customized payment plan, connecting them with financial counseling services, or explaining potential eligibility for assistance programs, all before they even receive a bill.
- Hyper-Personalization at Scale: The unified data approach allows for unparalleled personalization in patient communication. Instead of generic billing statements, AI can generate clear, concise explanations of benefits tailored to a patient’s specific procedure, insurance plan, and financial history. This level of personalized communication, facilitated by AI, reduces confusion, builds trust, and encourages timely payments, significantly enhancing the patient experience.
The Holistic Payoff: The Business Impact of a Unified RevOps Approach
Embracing an AI-powered, unified RevOps approach delivers a profound and measurable impact across the entire organization, moving beyond incremental improvements to achieve holistic transformation.
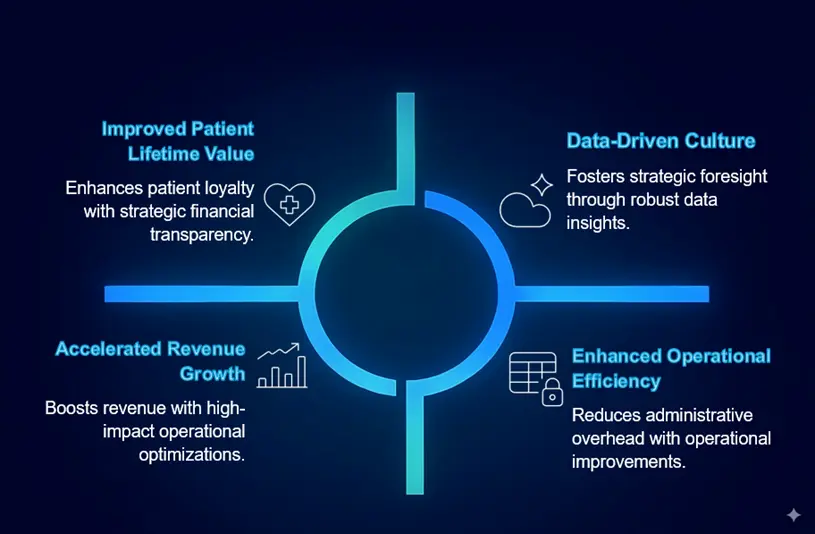
- Accelerated Revenue Growth: The most direct impact is a measurable increase in net revenue. By significantly reducing denial rates, optimizing claims processing, and improving payment capture, healthcare organizations experience a healthier bottom line and a more predictable revenue stream. This allows for strategic investments in patient care and facility upgrades.
- Enhanced Operational Efficiency: The elimination of manual rework, redundant data entry, and reactive problem-solving translates into substantial time and cost savings. Staff can redirect their efforts from administrative firefighting to higher-value activities, such as patient engagement and process optimization. This drives down administrative overhead and improves overall productivity.
- Improved Patient Lifetime Value: A seamless and transparent financial experience significantly boosts patient satisfaction and trust. Patients who understand their financial obligations and feel supported are more likely to return for future services, recommend the organization to others, and engage proactively in their care. This cultivates stronger patient loyalty and increases their lifetime value to the organization.
- Data-Driven Culture: The shift from gut-feel decisions to strategies backed by robust, real-time data is perhaps the most fundamental change. With AI providing actionable insights, leaders can make informed decisions about staffing, resource allocation, service line expansion, and payer contract negotiations. This fosters a culture of continuous improvement and strategic foresight across all departments.
The holistic payoff of an AI-unified RevOps approach extends beyond financial metrics, creating a more efficient, patient-centric, and resilient healthcare enterprise.
The Future is Unified: Embracing an AI-First RevOps Mindset
In the rapidly evolving healthcare landscape, an AI-driven, unified RevOps model is no longer a luxury—it is a competitive imperative. Organizations that continue to operate with siloed data and fragmented processes will struggle to keep pace with rising costs, evolving payer demands, and increasing patient expectations. Financial survival and sustainable growth hinge on the ability to harness data intelligently.
For those ready to embark on this transformative journey, the first step is often a strategic data audit. Identify the most significant disconnects between your EHR and RCM systems. Where are the biggest bottlenecks? Which data points are most frequently inconsistent? Pinpointing these areas will provide a clear roadmap for initial AI implementation and demonstrate early, tangible returns.
At OTLEN, we envision a future where synergy definitively replaces silos. A future where AI empowers a truly holistic approach to patient care and financial health. This is not merely about technology; it’s about redefining how healthcare operates, ensuring every patient interaction is seamless, every financial outcome is optimized, and every strategic decision is informed by intelligence. The future of healthcare operations is unified, and it is powered by AI.
