Executive Summary
Revenue leakage is a pervasive and costly challenge for the healthcare and biotech industries, with billions of dollars lost annually due to issues like coding errors, missed charges, and complex payer rules. This financial drain puts significant pressure on organizations already facing regulatory shifts and margin compression. A proactive, AI-powered pre-bill review process has emerged as a transformative solution. This acts as a “digital scalpel,” precisely identifying and correcting potential revenue leaks before claims are ever submitted. This preventative approach is the core differentiator in achieving financial integrity.
This white paper will explore the multifaceted problem of revenue leakage, detailing its impact on both traditional healthcare providers and the unique, high-stakes billing complexities of the biotech sector—from clinical trial billing to specialty drug reimbursement. We will examine how AI technologies, such as Natural Language Processing (NLP) and predictive analytics, are revolutionizing the pre-bill review process, leading to enhanced accuracy, operational efficiency, and regulatory compliance. Key takeaways include the significant potential for revenue recovery, drastically reduced denial rates, and a stronger financial foundation.
Adopting AI-powered pre-bill review is no longer just an option but a strategic imperative for financial health and sustainable growth.
Industry Context & Problem Statement
Revenue Leakage Defined: Revenue leakage in healthcare refers to the unforeseen loss of revenue that a provider has earned but not collected. Common sources of this leakage include inaccurate coding, missed charge capture, claim denials, and underpayments. While often addressed reactively through denial management, the most effective strategy is to prevent these issues from occurring in the first place through a robust pre-bill review. These leaks, though sometimes subtle, accumulate into substantial financial losses over time.
Biotech-Specific Challenges: The biotech industry faces unique and complex billing challenges that exacerbate revenue leakage. The intricate nature of clinical trials, gene therapies, and specialty drugs requires meticulous documentation and adherence to often-ambiguous billing codes. For instance, accurately capturing all billable services and supplies within a multi-phase clinical trial is a common failure point that AI can directly address. Furthermore, documenting medical necessity for novel treatments to ensure reimbursement is a process fraught with manual-review complexities that are prime candidates for automation. The pharmaceutical sector, a close counterpart to biotech, loses over $15 billion annually to revenue leakage, highlighting the scale of the problem.
Healthcare System Pressures: Healthcare organizations operate in an environment of immense pressure. Regulatory shifts, frequent payer audits, and shrinking profit margins make revenue integrity a top priority. Patent expirations on major drugs are expected to cost top pharmaceutical companies hundreds of billions, intensifying the need to capture all earned revenue. The administrative burden of billing, with its high potential for human error, makes manual, reactive processes increasingly unsustainable and underscores the need for a proactive pre-bill review strategy.

The Role of Pre-Bill Review: The Core Differentiator
Pre-bill review is the critical process of auditing claims for accuracy and completeness before they are submitted to payers. This proactive approach is the single most important step in preventing revenue loss, as it rectifies errors that would otherwise lead to denials, payment delays, and write-offs. It is the core differentiator between a reactive, high-cost revenue cycle and a proactive, high-efficiency one.
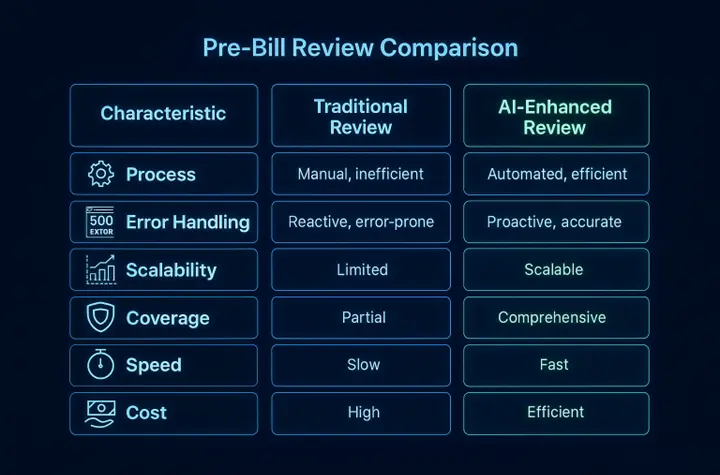
- Traditional Pre-Bill Review: Traditionally, this has been a manual, inefficient process. It relies on human auditors spot-checking a small percentage of claims, leaving significant revenue at risk due to the sheer volume of encounters that go unreviewed. This method is slow, prone to human error, and simply cannot scale to meet the complexities of modern healthcare and biotech billing.
- AI-Enhanced Pre-Bill Review: AI-powered solutions fundamentally transform this process. They can analyze 100% of encounters before billing, acting as a comprehensive safety net. These systems use sophisticated algorithms to flag potential errors, identify missed charges (such as a forgotten infusion administration code for a specialty biotech drug), and ensure compliance with payer-specific rules—all with unparalleled speed and accuracy.
AI-Powered Pre-Bill Review: The Digital Scalpel
AI-powered pre-bill review acts as a digital scalpel, precisely targeting and excising revenue leakage at its source.
Core Capabilities:
- NLP for Clinical Documentation Analysis: Natural Language Processing (NLP) is a key AI technology that interprets unstructured clinical data, such as physician’s notes and lab reports. In biotech, this is crucial for extracting evidence of medical necessity for a new immunotherapy directly from clinical notes, ensuring the claim is coded accurately and fully supported from the start.
- Predictive Analytics for Charge Capture: AI uses predictive analytics to identify patterns in historical data and flag potential missed charges. By analyzing services rendered against charges billed, the system can predict the likelihood of denial and suggest corrections. For a biotech company managing a complex drug regimen, it can flag if a required ancillary service was performed but not billed for.
- Rule-Based Engines for Payer Compliance: AI-driven rule-based engines stay current with the complex and ever-changing rules of thousands of payers. This ensures claims are compliant with each payer’s specific requirements, a critical function when billing for high-cost biotech therapies that are often subject to intense scrutiny.
Technology Stack: AI-powered pre-bill review solutions are designed to integrate seamlessly with existing Electronic Health Records (EHRs), billing platforms, and Revenue Cycle Management (RCM) tools. This integration allows for a smooth, automated workflow.
Accuracy & Speed: AI significantly improves audit precision and dramatically reduces turnaround times. By automating the review process, AI can analyze vast amounts of data in seconds. AI-powered coding has been shown to achieve accuracy rates of over 95%, leading to a substantial reduction in claim denials and a healthier revenue cycle.
Strategic Benefits for Healthcare & Biotech Organizations
Adopting an AI-powered pre-bill review strategy offers a wide range of benefits:
- Revenue Integrity: The most immediate benefit is a significant reduction in claim denials and underpayments. By ensuring all services are accurately coded and billed proactively, organizations can capture millions in previously lost revenue.
- Operational Efficiency: Automating the pre-bill review process streamlines workflows, freeing coders and billers to focus on complex cases. This can lead to a significant increase in productivity, with some hospitals reporting a 40% increase in coder productivity.
- Compliance & Risk Mitigation: AI-powered systems help ensure compliance with complex regulations and payer rules, reducing the risk of audit penalties. For biotech, this is especially critical when navigating the specific documentation requirements for drugs under Emergency Use Authorization (EUA) or other special designations.
- The Biotech Advantage: For biotech companies, this proactive approach is a game-changer. The technology helps navigate complex billing for specialty drugs and clinical trials, ensuring these high-cost, high-impact therapies are properly reimbursed and that revenue is not left on the table due to clerical errors.
Implementation Framework: A Strategic Overview
Deploying an AI-powered pre-bill review system is a strategic initiative that unfolds in distinct phases. This framework provides a high-level roadmap for leadership to follow.
- Phase 1: Assessment & Goal Setting: Begin by identifying key areas of revenue leakage and defining clear objectives. This could include reducing denial rates by a target percentage or increasing revenue capture for a specific service line, like a new biotech drug launch.
- Phase 2: Vendor Evaluation & Pilot Program: Carefully assess potential AI vendors based on their technology, integration capabilities, and expertise in your sector (e.g., biotech). Initiate a controlled pilot program to validate the solution’s impact on a specific subset of claims.
- Phase 3: Integration & Change Management: Integrate the AI solution with existing EHR and RCM systems. This phase requires strong stakeholder alignment—from RCM teams to clinicians—and comprehensive training to ensure user adoption and a smooth transition.
- Phase 4: Full-Scale Deployment & Optimization: Following a successful pilot, roll out the AI system across the organization. Continuously monitor key performance indicators and optimize the system to expand its impact.
For organizations ready to move from strategy to action, this framework serves as the foundation. A more detailed, tactical guide, our “No-Show Blueprint,” provides the granular, step-by-step details for a successful implementation and is the ideal next step for your operational teams.
Case Studies & Success Metrics
Real-world examples demonstrate the transformative impact of AI-powered pre-bill review:
- A large hospital system implemented an AI-powered pre-bill review solution and captured an additional $3-4 million per month in previously missed revenue.
- Auburn Community Hospital in New York saw a 4.6% increase in reimbursements and a 40% boost in coder productivity after adopting AI.
Key Performance Indicators (KPIs):
- Revenue Recovered: The amount of additional revenue captured proactively.
- Denial Rate Reduction: The percentage decrease in claim denials.
- First-Pass Resolution Rate (FPRR): The percentage of claims accepted on first submission.
Future Outlook
The role of AI in the revenue cycle is continuously evolving.
Emerging Trends:
- Generative AI: Generative AI is poised to further revolutionize medical billing by automating the creation of clinical documentation and billing codes from voice or text inputs. By 2026, many hospitals are expected to use Generative AI for these tasks.
- Real-Time Billing Validation: AI will enable real-time validation of billing information at the point of care, further embedding the pre-bill review concept directly into the clinical workflow.
- Payer Collaboration: Greater collaboration between payers and providers in implementing AI will be necessary to reduce administrative friction.
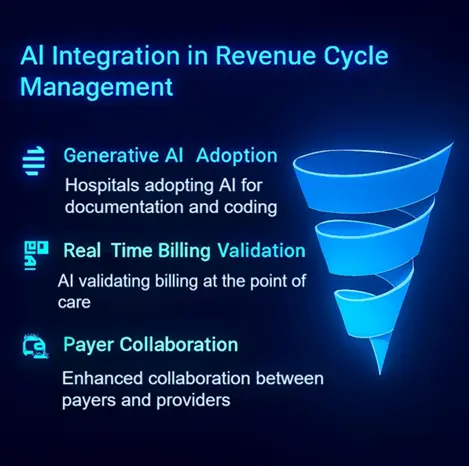
The Evolving Role of AI: AI is moving from a task-specific tool to the core infrastructure of revenue cycle management, enabling a more holistic and proactive approach to financial health.
Strategic Recommendations: Healthcare and biotech organizations should begin exploring AI solutions now to remain competitive. Starting with a strategic implementation of pre-bill review positions them for long-term financial success.
Conclusion & Call to Action
The healthcare and biotech industries can no longer afford the significant financial drain caused by revenue leakage. AI-powered pre-bill review offers a powerful and precise solution, enabling organizations to capture their rightfully earned revenue, improve operational efficiency, and mitigate compliance risks.
The evidence is clear: the technology has matured, the benefits are proven, and the strategic imperative is undeniable. Decision-makers who embrace this “digital scalpel” will not only carve out revenue leakage but also build a more resilient and financially sound future.
The next step is to schedule a personalized assessment with OTLEN to identify revenue leakage in your organization.
